


Hey everyone!
The new COVID-19 stuff:
Many countries have put their disagreements aside in joint effort to combat the virus – it is incredible what we are capable of if we work together..

This is all great information but…What I really wanted to share is why some COVID-19 patient are deteriorating rapidly, while others don’t even get symptoms, these are two extreme responses to the same virus.
The virus invades the body via mucosa membranes it gets into the cells of the lungs and replicates- it uses the angiotensin-converting enzyme 2 (ACE2), for cell entry (McLintosh, K, 2020). The actual virus (which is not a living thing), is a single strand molecule (RNA) called a genome, this one is a betacoronavirus. To put it simply, this virus enters cells through ACE2 sites, replicates and then kills the cells (McLintosh, K, 2020). Our body’s immune system responses to this invasion can be the major contributing factors to severe complications.
We all have a mucosal lining that works as a barrier to infections – this is called mucosal immunity. This mucosa is where our innate immune system resides, and it also houses our resident bacteria or microbia – when an invader comes in this mucosal membrane signals the cascades of the inflammatory and adaptive (cell-mediated) immune response.
Our non-specific innate immune response alerts of invaders using cytokines. If our mucosa is unable to keep the invaders at bay or if the immune system is dysregulated (autoimmune disease or compromised diseases) – they release more and more cytokines and this dysregulated response is unorganized. This can be problematic. Cytokine storms can occur from this and cause inflammation that lead to ruptured blood vessels that leak in to the systemic system. The virus can also move further down the respiratory tract as the immune response thus far is ineffective, this creates more cell death and more unorganized cell mediator release. The influx of disorganized inflammatory and immune cells attempting to rid the virus, end up clogging and creating exudate (pus) inside the lungs and surrounding areas. This pus can build up and becomes its own host of bacterial infection (Pneumonia). Then the blood cannot exchange oxygen in the lungs due to this. Acute respiratory distress syndrome (ARDS) is a major complication in patients with severe disease and can manifest shortly after the onset of difficulty breathing (McLintosh, K, 2020). Other scenarios have also been reported (eg. lack of surfactant and collapse of alveola).
In short, our innate immune system, the mucosal lining (and our lung microbia) and the cell lining of the lungs should be able to identify the virus and effectively keep it at bay until macrophages can be called in an organized fashion to eat the virus – before it enters into our blood, body and cells. This response is much more complex than this- but one important factor is that the Immune system response appropriately, in an organized fashion.
Gut microbiota play a protective role in our systemic immunity- the GUT and LUNG microbiota are linked, communicate and send immune boosting or immune suppressing messages via the “Gut-Lung Axis” (Anand & Mande, 2018; Bingula, 2017; Chung, 2017; Mathieu et al., 2018; ; O’Dwye et al., 2016; Schuijt et al., 2016). There is also a GUT – Brain axis (and skin connection too) – but we will cover that in another article.
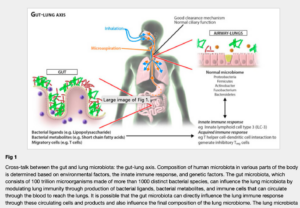
This GUT-LUNG axis is a communication of mediators AND actual movement of cells. These microorganisms and their parts within the lamina propria (GUT) are transferred to the mesenteric lymph nodes by antigen presenting cells (APCs) which can subsequently migrate out of the gut-associated lymphatic tissue (GALT) and reach both mucosal and peripheral non mucosal tissues of the lungs, including the bronchial epithelium (Clark et al, 2010; Bingula, 2017). Then they can modify the immune response and IMPROVE the immune response against pulmonary pathogens (Clark et al., 2010)- eg. COVID.
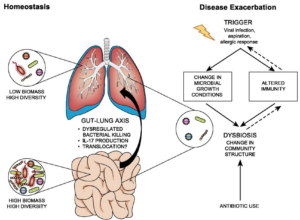
In other words, if your gut is in dysbiosis – your entire systemic immune system is affected. It also works in reverse – toxic intake into your lungs can cause issues in your Gut microbia.
Well the thing is you can have an unbalanced gut microbia and have very little symptoms (until it becomes very bad). Most of us just deal with faint nausea, constipation, diarrhea, bloating, acne, irritability, insomnia, fibromyalgia, etc. on a day to day basis. ALL of these have been linked to Dysbiosis of the GUT. So even with no major symptoms of underlying disease – you can have unbalanced GUT microbiota for years – this directly effects the organization, strength and abilities of your immune response.
(O’Dwyer et al., 2016)
HOW?
Many healthy and happy wishes,
Kaley
References:
Anand, S., & Mande, S. S. (2018). Diet, microbiota and gut-lung connection. Frontiers in microbiology, 9, 2147.
Bingula, R., Filaire, M., Radosevic-Robin, N., Bey, M., Berthon, J. Y., Bernalier-Donadille, A., … & Filaire, E. (2017). Desired turbulence? Gut-lung axis, immunity, and lung cancer. Journal of oncology, 2017.
Belcheva, A., Irrazabal, T., Robertson, S. J., Streutker, C., Maughan, H., Rubino, S., … & Green, B. (2014). Gut microbial metabolism drives transformation of MSH2-deficient colon epithelial cells. Cell, 158(2), 288-299.
Brown, E. M., Kenny, D. J., & Xavier, R. J. (2019). Gut microbiota regulation of T cells during inflammation and autoimmunity. Annual review of immunology, 37, 599-624.
Clarke, T. B., Davis, K. M., Lysenko, E. S., Zhou, A. Y., Yu, Y., & Weiser, J. N. (2010). Recognition of peptidoglycan from the microbiota by Nod1 enhances systemic innate immunity. Nature medicine, 16(2), 228.
Chung, K. F. (2017). Airway microbial dysbiosis in asthmatic patients: a target for prevention and treatment?. Journal of Allergy and Clinical Immunology, 139(4), 1071-1081.
Kim, C. H. (2016). B cell-helping functions of gut microbial metabolites. Microbial Cell, 3(10), 529.
Mathieu, E., Escribano-Vazquez, U., Descamps, D., Cherbuy, C., Langella, P., Riffault, S., … & Thomas, M. (2018). Paradigms of lung microbiota functions in health and disease, particularly, in asthma. Frontiers in physiology, 9, 1168.
McLintosh, K (2020). Coronavirus Disease 2019 (COVID-19). In Hirsch. M (Ed), UpToDate. Retrieved March 2020, from https://www.uptodate.com/contents/coronavirus-disease-2019-covid-19
O’Dwyer, D. N., Dickson, R. P., & Moore, B. B. (2016). The lung microbiome, immunity, and the pathogenesis of chronic lung disease. The journal of immunology, 196(12), 4839-4847.
Schuijt, T. J., Lankelma, J. M., Scicluna, B. P., e Melo, F. D. S., Roelofs, J. J., de Boer, J. D., … & de Vos, W. M. (2016). The gut microbiota plays a protective role in the host defence against pneumococcal pneumonia. Gut, 65(4), 575-583.
Shreiner, A. B., Kao, J. Y., & Young, V. B. (2015). The gut microbiome in health and in disease. Current opinion in gastroenterology, 31(1), 69.
Tian, S., Hu, W., Niu, L., Liu, H., Xu, H., & Xiao, S. Y. (2020). Pulmonary pathology of early phase 2019 novel coronavirus (COVID-19) pneumonia in two patients with lung cancer. Journal of Thoracic Oncology.