


Hello everyone! I know it has been a while, but I have been busy with helping some clients with some very interesting symptoms. The more and more I read about histamine, allergies and gut health, the more I am discovering about this interesting phenomenon.
Do these symptoms sound familiar to you?
Let’s start at the beginning:
Histamine is a biogenic amine that is naturally found in some foods and also produced by the body (Smolinska et al., 2014). Histamine and its 4 complex receptors represent a complex system of immunoregulation, they are thought to regulate both innate and adaptive immune response cells (Ferstl et al., 2012; Smolinska et al., 2014).
Histamine can have both pro-inflammatory and anti-inflammatory effects on immunoregulatory processes, depending on which histamine receptor is activated.
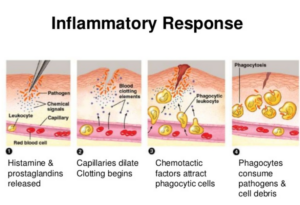
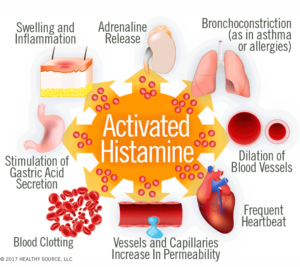
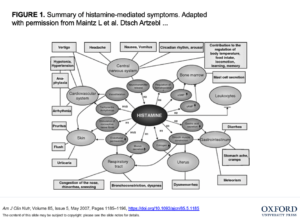
During an invasion from external pathogens histamine is released from Mast cells and other innate immune cells. This triggers smooth muscle contraction in the intestines (often causing cramps and diarrhea), expansion of blood vessels (causing low blood pressure), mucus secretion in the nasal passages and GI tract, and many other physiologic effects (allergy-like symptoms) that are intended to fight off invaders (Maintz & Novak, 2007).
Once the perceived threat is over, histamine levels are reduced back to normal, and symptoms subside. Normally the body has two enzymes that are capable of degrading histamine: N-methyltransferase (HNMT) and diamine oxidase (DAO) or it accumulates in the body.
Histamine is also released from cells in the stomach, where it triggers acid secretion from parietal cells, increasing the acidity of the stomach (Smolinska et al., 2014), which helps to fight off ingested pathogens.
Histamine is produced in the brain (specifically, in the tuberomammillary nucleus of the hypothalamus), where it acts as an excitatory neurotransmitter and plays a role in regulating the sleep-wake cycle (Scammell et., 2019).
Also, mast cells respond to neurotransmitters (in the brain) and synthesize and secrete molecules (histamine) that modulate neural responses as well (Corticotropin releasing hormone, serotonin, nerve growth factor, etc.) (Martinez et al., 2012).
Histamine intolerance is thought to result from an incorrect balance between accumulated histamine and the capacity for histamine degradation/breakdown (Smolinska et al., 2014; Pinzer et al., 2018)
This is a perpetual build-up of inflammatory and/or immune responses eventually causes symptoms that are very similar to an allergic reaction.
It is estimated that 1% of the population has histamine intolerance, and most of those are middle-aged women – 70% of histamine interlace is due to under active Diamine Oxidase (DAO). (Manzotti et al., 2016; Maintz & Noval, 2007).
Studies have shown that estrogen regulates histamine receptors in the brain, as well as liberates histamine release from mast cells (cells that exist in the lining of our tissues), and in contrast progesterone inhibits it (Vasiadi et al., 2006). Therefor, those experiencing estrogen dominance could be suffering from histamine intolerance as well.
As you can see, histamine and its receptors are responsible for many body functions:
They have found:
In the GI tract, mast cells (Mast cells synthesize Histamine) are activated during a stress response (any). Mast cells respond to and produce corticotropin-releasing hormone (Cortisol- Key modulator of Stress response) (Wallon et al., 2008). Upon activation they release numerous pro-inflammatory mediators (including histamine), similarly to the immune response (but there is not always a foreign invader).
Mast cell activation has been link with stress-induced mucosal barrier impairment (leaky gut), which in turn creates more mucosal inflammation (Martinez et al., 2012; Smolinska et al., 2014).
This is where the viscous circle begins…
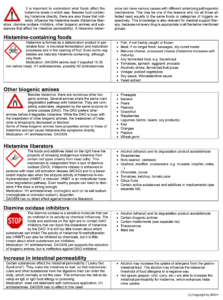
Stress, high histamine (biogenic amine) foods, and certain conditions (allergies etc.) can cause our immune system to release more histamine than is needed, which eventually leads to dysbiosis and leaky gut as it accumulates in the gut. It is ALSO suggested that people who already have dysbiosis (from other reasons- eg. antibiotics or candida overgrowth) are at high risk for developing histamine intolerance as our immune system is over stimulated.
The accurate diagnosis of histamine intolerance (HIT) should be based on the well-documented association between food consumption and symptoms, identification of food causing symptoms, determination of histamine content of the food causing the symptoms, exclusion of other causes (e.g., allergy, toxins, metabolites), oral histamine provocation (if possible), determination of DAO and HNMT contents and activity in intestinal mucosa (not in peripheral blood), and the analysis of DAO and HNMT genetic polymorphisms (Smolinska et al., 2014). There is no specific blood testing diagnostic tool for histamine intolerance, the span of time it takes for histamine to build up in the body is usually longer than what is allowed during testing (Kohn, 2014).
It is noted in the literature that the food industry needs to be more honest about the content of biogenic amines in foods and prevent patients’ misunderstanding (Martin & Garicano, 2016).

Optimizing gut bacteria is vital for overall health and disease prevention. Unfortunately, that’s not easy to do for those with histamine intolerance because probiotic foods (yogurt, kefir, kombucha, etc.) are high in histamine and should be avoided.
It’s important to choose probiotic supplements containing bacteria that do not produce histamine.
The following strains may be helpful because they have been found to break down (Biogenic Amines) or reduce the formation of histamine:
These strains should be avoided because they produce histamine in the GI tract:
See the photo from the Swiss Interest Group Histamine Intolerance for the foods that can be related to each of the histamine imbalances.

www.vitalityhealthsolutions.org
https://www.instagram.com/vitality_healthsolutions/
Copyright ©2020 VitalityHealthSolutions, All rights reserved.
References:
Bae, M. J., Shin, H. S., Chai, O. H., Han, J. G., & Shon, D. H. (2013). Inhibitory effect of unicellular green algae (Chlorella vulgaris) water extract on allergic immune response. Journal of the Science of Food and Agriculture, 93(12), 3133-3136.
Barcik, W., Pugin, B., Brescó, M. S., Westermann, P., Rinaldi, A., Groeger, D., … & Ferstl, R. (2019). Bacterial secretion of histamine within the gut influences immune responses within the lung. Allergy, 74(5), 899-909.
Esposito, F., Montuori, P., Schettino, M., Velotto, S., Stasi, T., Romano, R., & Cirillo, T. (2019). Level of biogenic amines in red and white wines, dietary exposure, and histamine-mediated symptoms upon wine ingestion. Molecules, 24(19), 3629.
Ferstl, R., Akdis, C. A., & O’Mahony, L. (2012). Histamine regulation of innate and adaptive immunity. Front Biosci, 17(1), 40-53.
Horny, H. P., Reiter, A., Sotlar, K., & Valent, P. (2018). Mastocytosis. In Encyclopedia of Pathology (pp. 1-11). Springer, Cham.
Kohn, J. B. (2014). Is there a diet for histamine intolerance?. Journal of the Academy of Nutrition and Dietetics, 114(11), 1860.
Liu, Q., Huang, Y., Zhang, R., Cai, T., & Cai, Y. (2016). Medical application of Spirulina platensis derived C-phycocyanin. Evidence-based complementary and alternative medicine, 2016.
Maintz, L., & Novak, N. (2007). Histamine and histamine intolerance. The American journal of clinical nutrition, 85(5), 1185-1196.
Martínez, C., González-Castro, A., Vicario, M., & Santos, J. (2012). Cellular and molecular basis of intestinal barrier dysfunction in the irritable bowel syndrome. Gut and liver, 6(3), 305.
Manzotti, G., Breda, D., Di Gioacchino, M., & Burastero, S. E. (2016). Serum diamine oxidase activity in patients with histamine intolerance. International journal of immunopathology and pharmacology, 29(1), 105-111.
Martin, I. S. M., Brachero, S., & Vilar, E. G. (2016). Histamine intolerance and dietary management: A complete review. Allergologia et immunopathologia, 44(5), 475-483.
Pinzer, T. C., Tietz, E., Waldmann, E., Schink, M., Neurath, M. F., & Zopf, Y. (2018). Circadian profiling reveals higher histamine plasma levels and lower diamine oxidase serum activities in 24% of patients with suspected histamine intolerance compared to food allergy and controls. Allergy, 73(4), 949-957.
Rahmani, J., Miri, A., Mohseni-Bandpei, A., Fakhri, Y., Bjørklund, G., Keramati, H., … & Khaneghah, A. M. (2018). Contamination and prevalence of histamine in canned tuna from Iran: a systematic review, meta-analysis, and health risk assessment. Journal of food protection, 81(12), 2019-2027.
Sánchez-Pérez, S., Comas-Basté, O., Rabell-González, J., Veciana-Nogués, M. T., Latorre-Moratalla, M. L., & Vidal-Carou, M. C. (2018). Biogenic Amines in Plant-Origin Foods: Are they Frequently Underestimated in Low-Histamine Diets?. Foods, 7(12), 205.
Scammell, T. E., Jackson, A. C., Franks, N. P., Wisden, W., & Dauvilliers, Y. (2019). Histamine: neural circuits and new medications. Sleep, 42(1), zsy183.
Schink, M., Konturek, P. C., Tietz, E., Dieterich, W., Pinzer, T. C., Wirtz, S., … & Zopf, Y. (2018). Microbial patterns in patients with histamine intolerance. J Physiol Pharmacol, 69(4), 579-593.
Smolinska, S., Jutel, M., Crameri, R., & O’mahony, L. (2014). Histamine and gut mucosal immune regulation. Allergy, 69(3), 273-281.
Vasiadi, M., Kempuraj, D., Boucher, W., Kalogeromitros, D., & Theoharides, T. C. (2006). Progesterone inhibits mast cell secretion. International journal of immunopathology and pharmacology, 19(4), 787-794.
Waldum, H. L., Brenna, E., Sandvik, A. K., & Prinz, C. (2000). The mechanism of histamine secretion from gastric enterochromaffin-like cells. American Journal of Physiology-Cell Physiology, 278(6), C1275-C1276.
Wallon, C., Yang, P. C., Keita, Å. V., Ericson, A. C., McKay, D. M., Sherman, P. M., … & Söderholm, J. D. (2008). Corticotropin-releasing hormone (CRH) regulates macromolecular permeability via mast cells in normal human colonic biopsies in vitro. Gut, 57(1), 50-58.